In Vitro Fertilization (IVF) is a promising fertility treatment that gives hope to those struggling to conceive naturally. It involves stimulating the ovaries to produce eggs, which are then fertilized in a lab before being implanted into the uterus. Women over 35, those dealing with endometriosis or polycystic ovary syndrome (PCOS), and couples facing male factor infertility are often prime candidates for IVF. A thorough evaluation by a specialist, including medical history and fertility tests, is necessary to see if IVF fits your situation. While it can significantly enhance conception chances, it’s important to approach treatment with realistic expectations and awareness of associated costs.
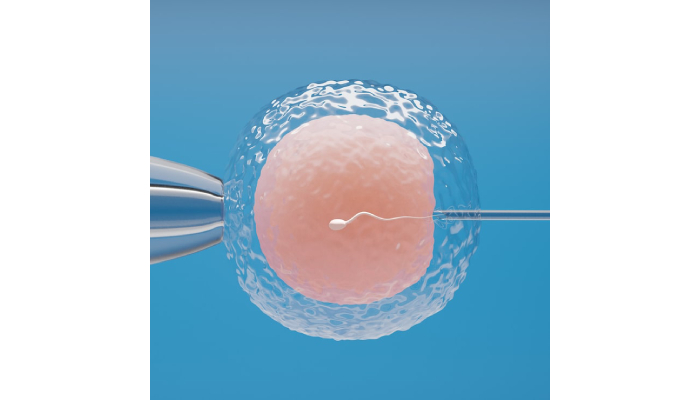
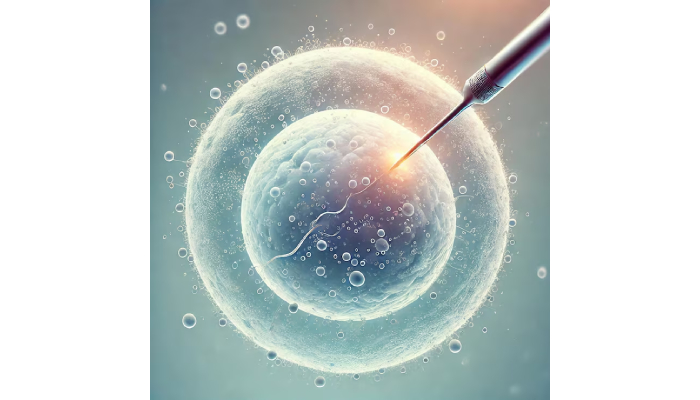
1. What is IVF and How Does It Work?
IVF San Diego, or In Vitro Fertilization, is an innovative fertility treatment that allows for fertilization to happen outside the body in a lab setting. The process kicks off with ovarian stimulation, where hormone injections are used to encourage the ovaries to produce multiple eggs. Once the eggs reach maturity, they are retrieved through a minor surgical procedure. These retrieved eggs are then combined with sperm in a controlled laboratory environment, where fertilization takes place. After fertilization, the embryos are carefully monitored for growth, typically over a period of 3 to 5 days, before one or more healthy embryos are selected for transfer into the uterus, aiming for successful implantation. If there are surplus embryos, they can be frozen for future use, increasing the chances of conceiving later on. Additionally, IVF can incorporate preimplantation genetic testing, allowing for the screening of genetic disorders before embryo transfer. The entire IVF journey spans several weeks, and some individuals may require multiple cycles to achieve success. This widely used assisted reproductive technology has transformed the lives of many couples, offering hope and a pathway to parenthood.
2. Who Are the Best Candidates for IVF?
When considering IVF, certain factors can help determine if you are a good candidate. Women over 35 often fall into this category, as age-related fertility decline can make natural conception more challenging. If a couple has been trying to conceive for over a year without success, or six months if the woman is older, they may qualify for IVF. Specific medical conditions can also make IVF a beneficial option. For instance, women with endometriosis might face difficulties due to adhesions, while those with Polycystic Ovary Syndrome (PCOS) may struggle with irregular ovulation. IVF provides a pathway for these women by allowing for direct fertilization and implantation. Additionally, blocked fallopian tubes greatly hinder natural conception, making IVF a practical solution as it bypasses these tubes entirely.
Moreover, male factor infertility, such as low sperm count, can prompt couples to explore IVF, particularly with techniques like Intracytoplasmic Sperm Injection (ICSI) enhancing the chances of fertilization. Couples dealing with unexplained infertility after thorough testing may also find IVF a viable option, as it can help tackle issues that remain unclear. If prior fertility treatments have not yielded positive results, IVF might be the next logical step. It’s also worth noting that IVF is accessible to single women and same-sex couples, allowing them to pursue their dreams of parenthood.
For those with a family history of genetic disorders, IVF offers the opportunity for genetic testing, ensuring healthier conception. Ultimately, the decision to pursue IVF should come after a comprehensive evaluation with a fertility specialist, who can assess individual circumstances and guide couples toward the best options.
3. Factors Influencing IVF Success Rates
Success rates for IVF can vary widely, and several key factors come into play. Age is one of the most significant, typically, younger women have higher success rates due to better egg quality and quantity. Moreover, the quality of both eggs and sperm plays a crucial role; higher quality gametes lead to more favorable outcomes. The number of embryos transferred also impacts success rates; while transferring more embryos can increase the chances of conception, it also raises the risk of multiples, which can complicate the pregnancy.
Interestingly, women who have had previous pregnancies, especially without fertility treatments, tend to have higher success rates with IVF. Lifestyle choices can’t be overlooked either; factors such as smoking, weight, and stress can significantly affect the effectiveness of the treatment. It’s also essential to consider any uterine abnormalities, as these can hinder implantation and overall success.
Additionally, underlying health issues, such as diabetes or thyroid disorders, must be managed to optimize IVF outcomes. The experience of the fertility clinic and the technology they use can greatly influence success rates, too. For example, genetic testing of embryos can help in selecting the healthiest ones, improving the chances of a successful pregnancy. Lastly, remember that individual responses to ovarian stimulation can vary, which impacts the number of viable eggs retrieved during the IVF process.
- Success rates can vary significantly based on age, with younger women typically having higher success rates.
- The quality of eggs and sperm plays a crucial role; higher quality gametes lead to better outcomes.
- The number of embryos transferred can influence success, with more embryos increasing chances but also higher risk of multiples.
- Previous pregnancies can improve success rates, especially if they were achieved without fertility treatments.
- Lifestyle factors like smoking, weight, and stress can impact the effectiveness of IVF.
- The presence of uterine abnormalities can affect implantation and overall success.
- Underlying health issues, like diabetes or thyroid disorders, need to be managed for optimal outcomes.
- The fertility clinic’s experience and technology used can significantly impact success rates.
- Genetic testing of embryos can improve the chances of a successful pregnancy by selecting the healthiest embryos.
- Individual response to ovarian stimulation can vary, affecting the number of viable eggs retrieved.
4. Common Medical Conditions That Qualify for IVF
Several medical conditions can make IVF a beneficial option for couples trying to conceive. For instance, endometriosis can cause significant scarring and inflammation, complicating natural conception. IVF offers a way around these challenges by allowing for direct embryo implantation into the uterus. Polycystic Ovary Syndrome (PCOS) often leads to irregular ovulation, but with IVF, doctors can help regulate and retrieve eggs effectively, increasing the chances of conception.
Blocked fallopian tubes are another common issue, as they prevent sperm from reaching the eggs. IVF completely bypasses this problem, allowing for fertilization outside the body. In cases of male factor infertility, like low sperm count or poor motility, IVF becomes necessary, frequently utilizing Intracytoplasmic Sperm Injection (ICSI) to enhance fertilization success.
Couples facing unexplained infertility after a year of trying, six months for those over 35, may find IVF to be a viable option, especially if initial fertility tests do not reveal clear issues. Additionally, those who have experienced recurrent pregnancy loss might seek IVF to maximize their chances of a successful pregnancy.
Certain genetic disorders also prompt the use of IVF, particularly when preimplantation genetic diagnosis is employed to prevent passing on inherited conditions. Other factors such as fibroids or uterine abnormalities can hinder natural conception, making IVF a practical alternative. Hormonal imbalances that disrupt ovulation can also lead to IVF being recommended, especially for women with a history of failed fertility treatments. In all these cases, IVF can provide a pathway to parenthood, tailored to individual medical needs.
5. The Importance of Ovarian Reserve Testing
Ovarian reserve testing is a key step in evaluating a woman’s fertility, especially for those considering IVF. This testing assesses both the quantity and quality of a woman’s eggs, which are vital for the success of the IVF process. Common methods include blood tests that measure hormone levels, such as Anti-Müllerian Hormone (AMH) and Follicle-Stimulating Hormone (FSH), as well as ultrasound assessments to count the number of follicles in the ovaries. A lower ovarian reserve can indicate a reduced chance of successfully retrieving and fertilizing eggs during IVF, making this information crucial for both patients and fertility specialists. Understanding one’s ovarian reserve allows for the customization of IVF protocols, optimizing hormone stimulation and egg retrieval strategies. This testing is particularly beneficial for women who may be contemplating the timing of IVF, as it can guide family planning decisions. For those with diminished ovarian reserve, egg freezing can be a valuable option if they wish to delay pregnancy. Additionally, the results from ovarian reserve testing can influence how many embryos are transferred during IVF and provide insights into the likelihood of requiring multiple IVF cycles. Ultimately, ovarian reserve testing is an essential part of the IVF evaluation process, empowering women with knowledge about their reproductive health and enhancing their chances of a successful pregnancy.
6. Understanding the IVF Evaluation Process
The IVF evaluation process is an essential first step for couples considering this path to parenthood. It all begins with a careful review of both partners’ medical histories to pinpoint any issues that might affect fertility. Following that, fertility tests are typically conducted for both partners, which may include blood tests, ultrasounds, and semen analysis. These tests help assess reproductive health and identify any underlying conditions that could impact IVF success.
One important aspect of the evaluation is imaging tests like hysterosalpingography. This test evaluates the health of the uterus and fallopian tubes, ensuring that the environment is conducive for embryo implantation. During this phase, doctors will also engage in conversations about personal goals and expectations, making sure that IVF aligns with the couple’s family-building plans.
Emotional readiness is another critical component, so counseling sessions may be recommended to help couples navigate the psychological aspects of IVF. Additionally, the medical team will provide a clear understanding of the IVF process, including potential risks and benefits, so patients can make informed decisions.
Lifestyle assessments may also be part of the evaluation, as factors like diet, exercise, and stress can all influence IVF success rates. For couples with a family history of genetic conditions, genetic counseling is often offered to discuss any risks involved. Finally, financial assessments are typically conducted to help couples understand the costs of treatment and explore their options for coverage. Overall, the evaluation aims to create a personalized treatment plan tailored to each couple’s unique needs.
7. Emotional and Financial Considerations for IVF
IVF can be an emotional rollercoaster, filled with moments of hope intertwined with anxiety and disappointment. Couples often find themselves on an unpredictable journey, making emotional support essential. Joining support groups or seeking counseling can provide valuable outlets for those navigating the ups and downs of IVF. The financial aspect of IVF is another significant consideration; the costs can be steep, ranging from $14,000 to $18,000, not including potential additional expenses for medications and genetic testing. Understanding insurance coverage and out-of-pocket costs is crucial for effective budgeting. Couples may want to explore financing options like loans or payment plans offered by clinics to manage this financial burden. It’s also vital to maintain transparency with the fertility clinic regarding costs to avoid unexpected expenses. Before starting IVF, couples should discuss and align their emotional and financial readiness, ensuring they have a solid support system in place to help manage both emotional and financial stresses during treatment.
8. Average Costs of IVF in San Diego
The average cost of a single IVF cycle in San Diego falls between $14,000 and $18,000, not including medications. This can quickly add up, especially if additional treatments like IUI or genetic testing are necessary. To make matters more complex, medications for ovarian stimulation can tack on another $3,000 to $5,000 to the total bill. Couples should also be aware that many clinics provide package deals, which can help lower costs for multiple cycles or additional services.
Geographical location plays a role in these expenses, as urban areas generally see higher price tags for healthcare services. Insurance coverage is another variable in this equation; some plans may cover IVF, while others do not, making it essential to verify benefits before moving forward. To ease the financial burden, some clinics and non-profits offer financial assistance programs. Payment plans or financing options can also be a lifesaver, making treatment more accessible for couples.
However, it’s crucial to discuss hidden costs upfront with the clinic, such as lab fees or charges for embryo freezing. Understanding the total financial commitment is vital for couples considering IVF in San Diego, as it can be a significant investment in their journey to parenthood.
9. Financing Options for IVF Treatment
Navigating the financial aspect of IVF treatment can be daunting, but many fertility clinics in San Diego offer financing options to ease this burden. Payment plans are commonly available, allowing couples to spread out costs over time, making it more manageable. Some clinics even partner with specialized financing companies that provide medical loans specifically for fertility treatments. Additionally, utilizing health savings accounts (HSAs) or flexible spending accounts (FSAs) can help cover IVF-related expenses tax-free, offering a smart way to save money while pursuing your dream of parenthood.
Crowdfunding has also gained popularity, allowing couples to raise funds through dedicated platforms designed for medical expenses. This community support can be a lifeline for many, bringing hope and financial relief. Moreover, certain non-profits and organizations provide grants or financial assistance for those who might find IVF costs overwhelming. It’s essential to research and compare the financing options available, as finding the right fit can make a significant difference in your journey.
Before committing to any financing agreement, understanding the terms, including interest rates, is crucial. Consulting with the clinic’s financial advisor can provide valuable insights into the best available options and potential savings. By establishing a clear financial plan, couples can alleviate stress and focus more on the emotional aspects of their IVF journey, paving the way toward their dream of starting a family.
10. Insights on Unexplained Infertility and IVF
unexplained infertility can be a challenging and often frustrating journey for couples trying to conceive. It affects a significant percentage of couples, leaving them without clear answers even after thorough testing. When standard tests do not reveal a reason for difficulty in conception, many feel lost. This is where IVF (In Vitro Fertilization) can shine as a beacon of hope. By directly addressing the fertilization and implantation processes, IVF bypasses potential unknown issues that may be hindering natural conception. While success rates for IVF in cases of unexplained infertility can vary, many couples find renewed hope in this treatment option.
Furthermore, genetic testing during IVF can uncover hidden issues that might not have been evident in prior evaluations. Couples are encouraged to engage in open communication with their fertility specialists, sharing concerns and questions to feel more informed and empowered throughout their journey. Emotional support plays a crucial role as well; counseling and support groups can help individuals navigate the emotional rollercoaster that often accompanies unexplained infertility. Additionally, making lifestyle modifications, such as improving diet and exercising, can also enhance fertility and may lead to better outcomes during the IVF process. Ultimately, many couples discover that IVF can open new doors to parenthood, even when the cause of infertility remains a mystery.